Blood clotting is pointed out as one of the main reasons for death in Covid-19 infected patients. Then question arises that what happens when corona virus infects to a person whose blood doesn’t coagulate easily? What will be the overall effect of Covid-19 on patients with blood clotting disorders like hemophilia?
What is hemophilia?
Hemophilia is a rare hereditary disorder, generally found in males, that reduces the blood’s ability to clot. People with hemophilia do not have enough clotting factors (most often factor VIII, or FVIII), so they bleed for a longer time than usual.
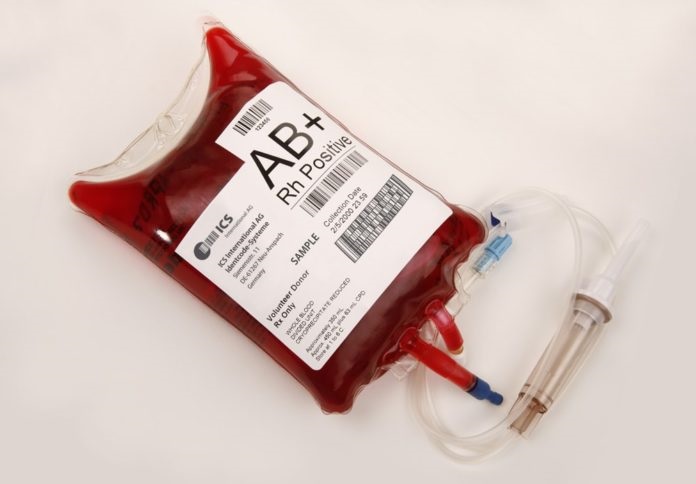
When injuries happen, blood thickens or coagulates to prevent excessive bleeding through a process termed hemostasis. Blood cells called platelets work with proteins (clotting factors) in blood plasma (the clear liquid) to form a clot over the wound to stop bleeding.
What is Covid infection’s impact on hemophiliacs?
Medical advisers say the risk for hemophiliacs is similar to healthy people, who doesn’t have any underlying medical conditions. They should follow the guidelines and prevent exposure to the virus.
If a person with hemophilia contracts Covid -19, they should follow the treatments prescribed to healthy people. But if the person is taking immunosuppressants, that would put them in the high-risk category. Also, there is a likelihood of getting acquired hemophilia A (AHA).
Patients with HIV (the virus that causes AIDS) and people with inhibitors who are on immunosuppressants are susceptible to complications arising from Covid-19 infections. Otherwise, the virus does not increase the chances of Covid-19 infection for patients with hemophilia and other bleeding disorders.
A Covid-19 infection and its accompanying stress can trigger the development of inhibitors even in patients without hemophilia, the Coalition for Hemophilia B says. So, patients have to be continually monitored as previously eliminated inhibitors can to be reactivated.
Is the swab test for Covid vulnerable for hemophiliacs?

A nasal or throat swab test for Covid-19 is not a potential trigger to bleed for hemophiliacs, if the patient hasn’t experienced any recent episode of nosebleed. But it’s advisable to inform the medical staff of the bleeding disorder so that they can assess the risk of a bleeding episode.
Know more about Covid tests in uae24x7.com
Covid-19 leads to Acquired Hemophilia?
A SARS-CoV-2 infection can result in acquired hemophilia A (AHA. AHA is an autoimmune disease in which the immune system produces antibodies that destroy a blood-clotting protein (factor VIII). It leads to blood clotting problems and bleeding that are similar to the symptoms of hemophilia A.
What is Acquired Hemophilia?
This is not one of the main types of hemophilia since it not caused by inherited gene mutations. This rare condition, usually witnessed in adulthood, is characterised by excessive bleeding into the skin, muscles, or soft tissues.
Acquired hemophilia results in auto-antibodies attacking and disabling the coagulation factor VIII. These auto-antibodies are usually associated with pregnancy, immune system disorders, cancer, or allergic reactions to certain drugs. In many other cases, the cause is unknown.
AHA tends to occur in the elderly, even those who do not have underlying medical conditions.
How is hemophilia treated?
The treatment for hemophilia may vary according to the severity of its condition. The two main approaches are preventative treatment and on-demand treatment.
- Preventative treatment: Clotting factor medicine is regularly injected to prevent bleeding and damage to joints and muscles. Most cases of hemophilia are severe and need preventative treatment. Preventative treatment is usually life-long.
- On-demand treatment: where medicine is used to treat prolonged bleeding.




![The Top & Most Popular Seafood Bucket Restaurants in Dubai for you [Never Miss]](https://uae24x7.com/wp-content/uploads/2020/09/8-seafood-in-a-bucket-scaled-e1600739237403.jpg)
![Procedures for Renewing the Driving License in Abu Dhabi [3 Simple Steps]](https://uae24x7.com/wp-content/uploads/2020/07/Capture-9-e1595666454466.jpg)